The benefits of breastfeeding in meeting the nutritional and health needs of infants and their mothers are well recognized (Victora et al., 2016; World Health Organization, 2003). According to a joint Global Strategy for Infant and Child Feeding by the World Health Organization (WHO) and the United Nations Children’s Fund (UNICEF), breastfeeding is of significant importance in ensuring that children meet their nutritional needs to allow for optimal development (World Health Organization, 2003).
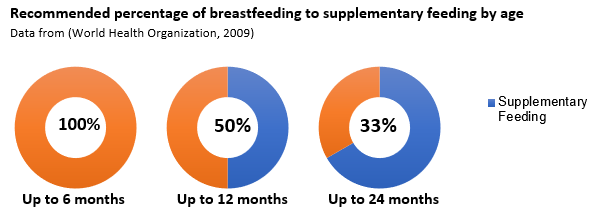
In the majority of cases, children should be exclusively breastfed for the first six months (World Health Organization, 2003) as breast milk provides all the nutrients and energy for a child’s growth, development and health (Binns et al., 2020). After these first six months, breastfeeding should continue alongside supplementary foods until a child is two years old (Binns et al., 2020). The image below outlines these recommendations.
Health Benefits of Breastfeeding:
Children who are breastfed experienced improved health compared to their peers. A meta-analysis published in The Lancet by Victora et al. (2016) identified that breastfeeding was correlated with a reduction in childhood infections and an increase in intelligence. Additionally, a Cochrane systematic review by McFadden et al. (2017) identified a reduced risk of overweight and the development of diabetes.
Breastfeeding also has significant health benefits for nursing mothers including reduced risk of breast and ovarian cancer (McFadden et al., 2017).
WHO and UNICEF Recommendations:
The Global Strategy for infant and young child feeding sets out recommendations to ensure optimal child feeding. These recommendations include:
- Exclusive breastfeeding to 6 months of age (World Health Organization, 2003)
- Supplemented breastfeeding supplemented with safe foods that provide adequate nutrition to 24 months of age or beyond (World Health Organization, 2003)
This Global Strategy also supports health system strengthening in the areas of health promotions and health sector availability in order to inform, build skills and confidence and address breastfeeding problems and concerns (World Health Organization, 2003).
In addition to this strategy, in 2012 the 56th World Health Assembly set a global target to achieve an exclusive breastfeeding rate of 50% for the first 6 months of life (McFadden et al., 2017).
Global Trends in Breastfeeding:
Despite the significant and well-accepted health benefits associated with breastfeeding, the rates of exclusive breastfeeding in the first 6 months are low. In 2016, the rate of exclusive breastfeeding in low- and middle-income countries was below 37% (Victora et al., 2016).
Interestingly, in low-income counties breastfeeding rates are affected by late initiation and low rates of exclusive breastfeeding while in middle- and high-income countries, breastfeeding duration is shorter (McFadden et al., 2017)
Breastfeeding in Viet Nam:
In Viet Nam, health authorities have promoted breastfeeding since the 1980s with a clear policy to encourage exclusive breastfeeding to 6 months and initiation of breastfeeding within the first hour of life (Thu et al., 2012). With the large majority (94% in 2014) of deliveries in Viet Nam occurring in institutional settings (UNICEF & WHO, 2018) the country has a opportunity for disseminating breastfeeding knowledge and resources.
Viet Nam has one of the lowest rates of breastfeeding in South East Asia (UNICEF, 2016) and the rates of early initiation have dropped from 44% (2006) to 27% (2014) over a period of 8 years (UNICEF & WHO, 2018).
Additionally, the rate of exclusive breastfeeding in Viet Nam was only 19.6% (CDC, 2019), which has not improved attributably to some extent to the aggressive marketing and widespread availability of breastmilk substitutes (BMS) (NIN, 2017). This rate also varies considerably between urban areas (30%) and rural and mountainous areas (70%) (Vietnam Women’Union, 2010).
This study:
There is currently no available evidence directly evaluating the national legislation around breastfeeding and the Breast Milk Substitutes Code (BMS Code), and the associated impact on community behavior and breastfeeding rates throughout Viet Nam. As such, a study is required to identify and evaluate the effectiveness of policy interventions in Viet Nam to address the structural determinants of breastfeeding.
The Research and Training Centre for Community Development (RTCCD) conducted such a study with financial support from FHI360.
Titled “Assessing the effectiveness of policies relating to breastfeeding promotion, protection and support in Viet Nam”, this study aims to build on the available evidence base and thereby advocate for stronger policies and improved enforcement in regards to breastfeeding and the BMS code.
This is achieved by assessing the potential impact of these policies and bottlenecks for successful implementation through the perspective of various stakeholders including policy makers, implementers, and beneficiaries.
The study is based on 4 main objectives:
- Review the availability and contents of BMS Code policies in Vietnam
- Review the implementation, coverage, monitoring and enforcement of these policies
- Examine the potential impact of these policies on pregnant and post-partum mothers in the Vietnamese community
- Explore the perceptions of stakeholders and beneficiaries in regards to these policies
This study was conducted from December 2019 to July 2020 and utilized a cross-sectional approach with both quantitative with qualitative methods. A sample size of 990 women was achieved, including pregnant women and women with children aged 0-12 months from 3 provinces: Bac Ninh, Binh Duong, and Ho Chi Minh City.
Findings obtained for this study are expected to be published in two articles in December 2020. These are:
- Exposure to powder milk during pregnancy and the post-partum period
- Maternity leave policy: from legislation to implementation
Follow the RTCCD website and fanpage for updates on the availability of this research.
For further information, please email Van Nguyen van.nguyen@rtccd.org.vn or Ha Tran ha.tran@rtccd.org.vn at RTCCD.
Some pictures of the data collection process:
References:
Binns, C., Lee, M. K., Yun Low, W., Baker, P., Bulgiba, A., Dahlui, M., . . . Tang, L. (2020). Guidelines for Complementary Feeding of Infants in the Asia Pacific Region: APACPH Public Health Nutrition Group. Asia Pacific Journal of Public Health, 32(4), 179-187. doi:10.1177/1010539520931328
CDC (2019). Sữa mẹ là nguồn dinh dưỡng tốt nhất cho sự phát triển của trẻ. Retrieved from http://ytdphanoi.gov.vn/720n/sua-me-la-nguon-dinh-duong-tot-nhat-cho-su-phat-trien-cua-tre.html.
McFadden, A., Gavine, A., Renfrew, M. J., Wade, A., Buchanan, P., Taylor, J. L., . . . et al. (2017). Support for healthy breastfeeding mothers with healthy term babies. Cochrane Database of Systematic Reviews(2). doi:10.1002/14651858.CD001141.pub5
Thu, H. N., Eriksson, B., Khanh, T. T., Petzold, M., Bondjers, G., Kim, C. N. T., . . . Ascher, H. (2012). Breastfeeding practices in urban and rural Vietnam. BMC Public Health, 12, 964-964. doi:10.1186/1471-2458-12-964
UNICEF, & WHO. (2018). Capture the moment – Early initiation of breastfeeding: The best start for every newborn. New York: UNICEF.
UNICEF (2016). Tỷ lệ nuôi con bằng sữa mẹ vẫn ở mức thấp. Retrieved from https://vietnammoi.vn/ty-le-nuoi-con-bang-sua-me-van-o-muc-thap-64825.htm.
Victora, C. G., Bahl, R., Barros, A. J. D., França, G. V. A., Horton, S., Krasevec, J., . . . Rollins, N. C. (2016). Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. The Lancet, 387(10017), 475-490. doi:10.1016/S0140-6736(15)01024-7
Vietnam Women’Union (2010). Tỷ lệ bà mẹ cho con bú ở thành thị thấp hơn nông thôn. Retriveved from http://hoilhpn.org.vn/web/guest/tin-chi-tiet/-/chi-tiet/nuoi-con-bang-sua-me-thanh-thi-thap-hon-nong-thon-14345-201.html
World Health Organization. (2003). Global Strategy for Infant and Young Child Feeding Geneva, Switzerland Retrieved from https://apps.who.int/iris/bitstream/handle/10665/42590/9241562218.pdf;jsessionid=23D30B37443F22E904EF54CF67885BEA?sequence=1.
World Health Organization. (2009). Infant and young child feeding: Model Chapter Geneva; Swizerland Retrieved from https://www.who.int/nutrition/publications/infantfeeding/9789241597494/en/.